Introduction
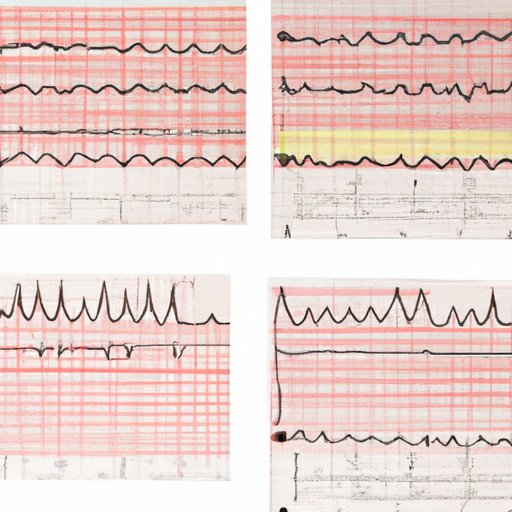
An EKG is a non-invasive diagnostic test that measures the electrical activity of your heart and records it as a series of waves. The test is painless and involves placing electrodes on your chest, arms, and legs, which then transmit the electrical signals to the EKG machine. EKG tracings provide valuable information for diagnosing various cardiac conditions, including arrhythmias, ischemia, and myocardial infarctions.
Regardless of your level of expertise, interpreting EKG results requires both knowledge of the basic principles behind EKG and a keen eye to recognize abnormalities. In this article, we will provide a detailed guide on how to read EKG, beginning with the basics and advancing to more complex EKG patterns. We will also explore the anatomy of the heart and how it correlates with EKG tracings, common EKG abnormalities and their clinical significance, and recent advancements in EKG technology that have transformed cardiac diagnosis and treatment.
Step-by-Step Guide on Interpreting EKG Results for Beginners
If you are new to EKG interpretation, it can seem overwhelming at first. However, with a little practice and guidance, you can quickly become proficient in interpreting EKG tracings. Here are the basic steps to follow:
Definition and Purpose of EKG
Before diving into EKG interpretation, it’s essential to understand what it is and why it’s important. An EKG is a graphical representation of the electrical activity of the heart. This electrical activity is generated by specialized cells in the heart known as pacemaker cells. These cells initiate and coordinate the contraction of the heart muscle, which pumps blood throughout the body.
The EKG machine records the electrical activity of the heart and produces a visual representation of this activity in the form of a waveform. The waveform reflects the depolarization and repolarization of the cardiac muscle, which generates the electrical impulses that coordinate the contraction of the heart.
EKG is essential in the diagnosis and management of various cardiac conditions. It can help detect arrhythmias, myocardial infarction, electrolyte imbalances, drug toxicity, and other conditions that affect the heart’s electrical activity.
Understanding the Basic Components of EKG Tracings
To interpret EKG tracings, you need to understand the basic components of the waveform. EKG tracings consist of several waves and segments, each of which represents a different aspect of the cardiac cycle. Here are the basic components of an EKG tracing:
P wave
The P wave represents the depolarization of the atria, which precedes atrial contraction. The P wave is characterized by a small, smooth wave that usually appears before the QRS complex.
QRS complex
The QRS complex represents the depolarization of the ventricles, which precedes ventricular contraction. The QRS complex is a larger, more complex waveform than the P wave, with three distinct deflections called the Q, R, and S waves.
T wave
The T wave represents the repolarization of the ventricles, which returns the cardiac muscle to its resting state. The T wave is a smooth, rounded wave that follows the QRS complex.
ST segment
The ST segment is a flat section of the EKG tracing that appears after the QRS complex and before the T wave. The ST segment represents the time when the ventricles are depolarized but not yet repolarized. It’s an essential segment to evaluate for myocardial ischemia and infarction.
How to Read and Interpret EKG Waveforms
Once you understand the basic components of EKG tracings, you can start interpreting them. Here are the basic steps to follow:
Step 1: Determine the heart rhythm
The first step in EKG interpretation is to determine the heart rhythm. This involves examining the intervals between consecutive R waves (RR intervals). If the RR intervals are regular, the rhythm is said to be sinus. Sinus rhythm is the normal rhythm of the heart and indicates proper electrical function. If the RR intervals are irregular, the rhythm is said to be irregular.
Step 2: Evaluate the P wave
The next step is to evaluate the P wave. The P wave should be upright, consistent in morphology, and precede each QRS complex. An absent P wave can indicate atrial fibrillation, while an enlarged P wave can indicate atrial hypertrophy.
Step 3: Examine the QRS complex
The QRS complex represents ventricular depolarization. The complex should be narrow, with a duration of less than 0.12 seconds. A wider QRS complex can indicate ventricular conduction abnormalities or bundle branch block.
Step 4: Evaluate the ST segment
The ST segment is a crucial segment to evaluate for myocardial ischemia and infarction. The ST segment should be flat and level with the baseline. An elevated ST segment can indicate myocardial infarction, while a depressed ST segment can indicate ischemia.
Common Mistakes and Pitfalls to Avoid When Interpreting EKG Results
Even experienced healthcare professionals can make mistakes when interpreting EKG results. Here are some common mistakes to avoid:
Mistake 1: Overreliance on EKG
EKG is an essential tool for cardiac diagnosis and management. However, it should be used in combination with other diagnostic tools, such as physical exam findings, patient history, and biomarkers. Overreliance on EKG can lead to missed diagnoses and inappropriate treatment decisions.
Mistake 2: Misinterpreting artifacts as abnormalities
EKG tracings can be affected by various artifacts, such as muscle tremors and electrode placement errors. These artifacts can mimic abnormal waveforms and lead to misinterpretation. It’s essential to recognize and differentiate between artifacts and true abnormalities.
Mistake 3: Failing to evaluate the clinical context
EKG interpretation should always consider the clinical context, including physical exam findings and patient history. For example, the presence of ST segment elevation may not necessarily indicate myocardial infarction if it’s not consistent with the patient’s symptoms or history.
A Comprehensive Overview of EKG Reading Techniques for Healthcare Professionals
Healthcare professionals who work with cardiac patients require a more advanced understanding of EKG interpretation beyond the basics. Here are some essential techniques for advanced EKG interpretation:
Beyond the Basics: Advanced EKG Techniques for Healthcare Professionals
Advanced EKG techniques include evaluating the T wave morphology and assessing the QT interval. The T wave morphology can provide important diagnostic clues for various cardiac conditions, while the QT interval can indicate risk for ventricular arrhythmias.
Strategies for Interpreting Complex EKG Patterns
Some EKG patterns can be quite complex and challenging to interpret. Strategies for interpreting complex EKG patterns include comparing the current EKG to previous EKGs, evaluating the clinical context, and consulting with other healthcare professionals for a second opinion.
How to Evaluate EKG Results in the Context of Patient History, Symptoms, and Physical Exam Findings
To improve the accuracy of EKG interpretation, healthcare professionals should always consider the patient’s history, symptoms, and physical exam findings. For example, a patient with chest pain and ST segment elevation is more likely to have myocardial infarction than a patient with ST segment elevation without symptoms or history of cardiac disease.
Challenges and Limitations of EKG Interpretation
EKG interpretation is not without limitations and challenges. These include variations in EKG morphology among individuals, limitations in detecting non-cardiac abnormalities, and the potential for misinterpretation and overdiagnosis.
Understanding the Anatomy of the Heart and How It Correlates to EKG Tracings
Understanding the anatomy of the heart is essential for EKG interpretation. Here are some key aspects of cardiac anatomy and their correlation to EKG tracings:
Overview of the Heart’s Electrical System
The heart’s electrical system consists of specialized cells that generate and conduct electrical impulses. The system includes the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers. These cells generate the electrical impulses that coordinate the contraction of the heart and generate EKG tracings.
How Cardiac Anatomy Affects EKG Waveforms
The location of the heart’s electrical system affects EKG waveforms. For example, the depolarization of the atria generates the P wave, while the depolarization of the ventricles generates the QRS complex. If there are abnormalities in the electrical system, it can alter EKG waveforms and indicate cardiac dysfunction.
Common EKG Abnormalities Related to Specific Areas of the Heart
Specific EKG abnormalities can indicate abnormalities or dysfunction in specific areas of the heart. For example, ST segment elevation in specific leads can indicate myocardial ischemia or infarction in specific areas of the heart. Recognizing these patterns can help healthcare professionals make accurate diagnoses and develop appropriate treatment plans.
Common EKG Abnormalities Explained and Their Clinical Significance
Here are some common EKG abnormalities and their clinical significance:
Examples of Common EKG Abnormalities
- Atrial fibrillation: Absent P waves and irregularly irregular rhythm
- Myocardial infarction: ST segment elevation in specific leads
- Ventricular tachycardia: Wide QRS complexes and rapid heart rate
- First-degree AV block: Prolonged PR interval
How to Recognize These Abnormalities on EKG Tracings
Recognizing abnormalities on EKG tracings requires familiarity with normal EKG patterns and the ability to differentiate between normal and abnormal waveforms. Healthcare professionals should always compare the current EKG to previous EKGs to detect changes in EKG patterns that indicate abnormalities.
Clinical Implications and Treatment Options for Each Abnormality
The clinical implications and treatment options for each EKG abnormality depend on the specific diagnosis. Atrial fibrillation, for example, may require anticoagulation therapy and rate control medication, while myocardial infarction may require invasive procedures such as angioplasty or thrombolytic therapy.
Advancements in EKG Technology and Their Impact on Cardiac Diagnosis and Treatment
Recent advancements in EKG technology have revolutionized cardiac diagnosis and management. Here are some examples of new EKG technologies and their impact:
Overview of New EKG Technologies and Techniques
New EKG technologies include mobile EKG devices, integrated EKG systems, and wearable EKG monitors. These devices can obtain EKG tracings quickly and accurately, allowing for faster diagnosis and management of cardiac conditions.
How These Advancements Have Improved Cardiac Diagnosis and Treatment
Advancements in EKG technology have improved cardiac diagnosis and treatment by allowing for faster and more accurate diagnosis, reducing healthcare costs, and improving patient outcomes. For example, wearable EKG monitors can detect arrhythmias that may not be captured during standard EKG tests.
Future Trends and Emerging Technologies in EKG
The future of EKG technology is focused on developing more portable and accurate devices and improving data analysis and interpretation. Emerging technologies include artificial intelligence and machine learning algorithms that can analyze EKG tracings and identify abnormalities more precisely.
Conclusion
In conclusion, EKG interpretation is a vital skill for healthcare professionals. Whether you are a beginner or a seasoned professional, accurately reading and interpreting EKG tracings requires knowledge of the basic principles behind EKG, a keen eye for abnormalities, and an understanding of how cardiac anatomy affects EKG waveforms. By following the steps outlined in this article, you can become proficient in EKG interpretation and help diagnose and manage various cardiac conditions.
Remember, EKG interpretation is just one tool in the arsenal of cardiac diagnosis and management. As such, always consider the clinical context, evaluate the patient’s history and symptoms, and consult with other healthcare professionals as needed.





